‘Time to focus on the blue dots’: an RCP workshop discussion on the NHS shift from hospital to community
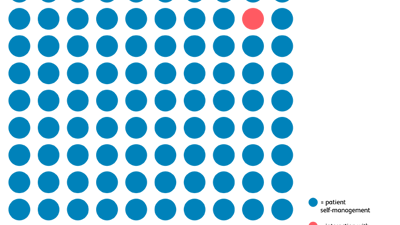
In April 2025, the RCP hosted a workshop that explored how the NHS can respond to the government’s promised ‘hospital to community’ shift in care – the so-called ‘left shift’. With over 40 participants, including clinicians, patient representatives, national charities, royal colleges and policymakers, the event has resulted in a new toolkit – Time to focus on the blue dots – which calls for a fundamental shift in how the NHS delivers care.